Search
- Page Path
- HOME > Search
Original Articles
- Clinical Study
- Achievement of LDL-C Targets Defined by ESC/EAS (2011) Guidelines in Risk-Stratified Korean Patients with Dyslipidemia Receiving Lipid-Modifying Treatments
- Ye Seul Yang, Seo Young Lee, Jung-Sun Kim, Kyung Mook Choi, Kang Wook Lee, Sang-Chol Lee, Jung Rae Cho, Seung-Jin Oh, Ji-Hyun Kim, Sung Hee Choi
- Endocrinol Metab. 2020;35(2):367-376. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.367
- 8,017 View
- 144 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study assessed the proportion of risk-stratified Korean patients with dyslipidemia achieving their low-density lipoprotein cholesterol (LDL-C) targets as defined by the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) (2011) guidelines while receiving lipid-modifying treatments (LMTs).
Methods
In this multicenter, cross-sectional, observational study, we evaluated data from Korean patients aged ≥19 years who were receiving LMTs for ≥3 months and had an LDL-C value within the previous 12 months on the same LMT. Data were collected for demographics, cardiovascular (CV) risk factors, medical history, and healthcare consumption. Patients were risk-stratified according to the ESC Systematic COronary Risk Evaluation (SCORE) chart and LDL-C target achievement rate was assessed.
Results
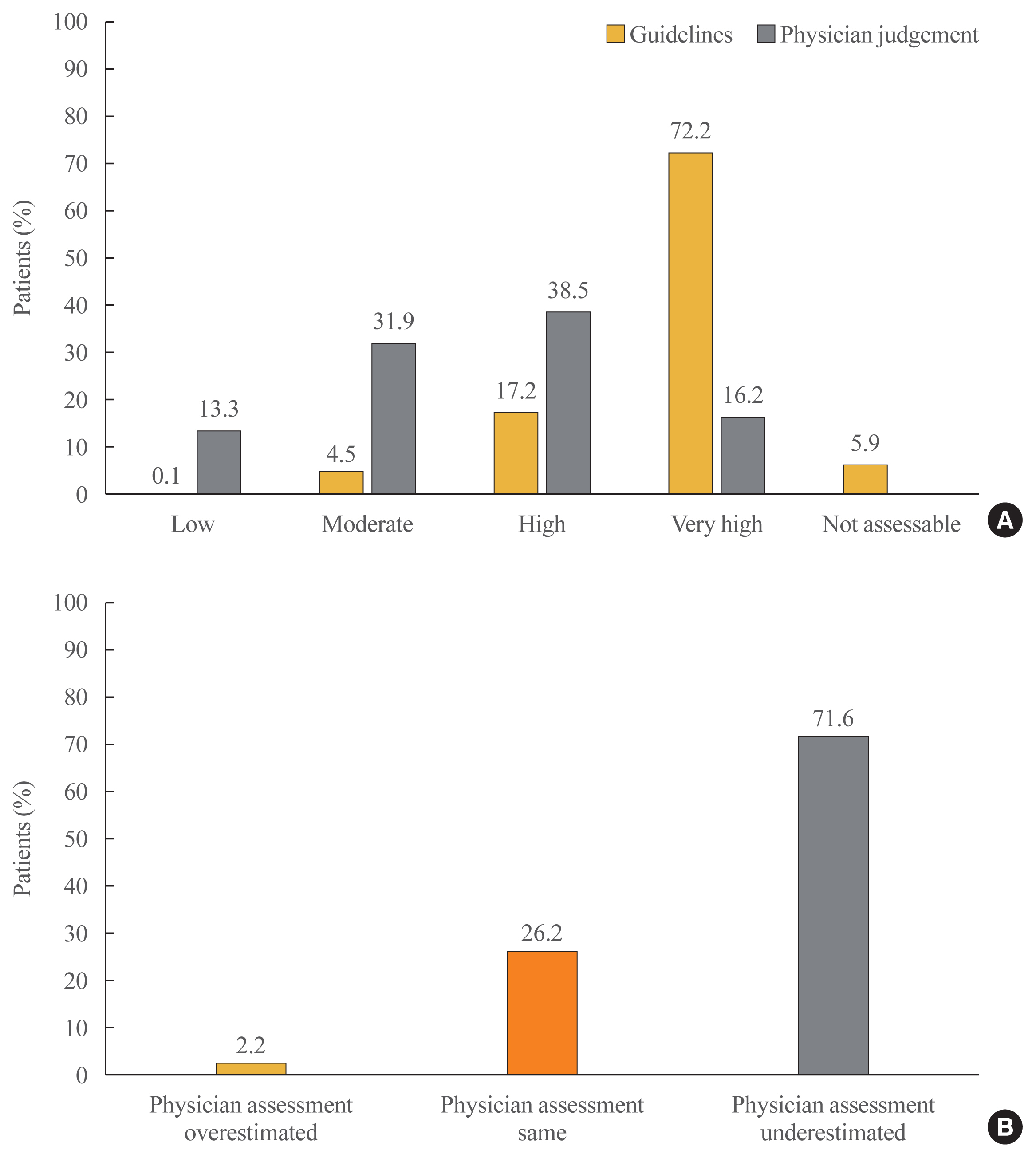
Guideline-based risk-stratification of the 1,034 patients showed the majority (72.2%) to be in the very high-risk category. Investigators’ assessment of risk was underestimated in 71.6% compared to ESC/EAS guidelines. Overall LDL-C target achievement rate was 44.3%; target achievement was the highest (66.0%) in moderate-risk patients and the lowest (39.0%) in very high-risk patients. Overall 97.1% patients were receiving statin therapy, mostly as a single-agent (89.2%). High-intensity statins and the highest permissible dose of high-intensity statins had been prescribed to only 9.1% and 7.3% patients in the very high-risk group, respectively. Physician satisfaction with patients’ LDL-C levels was the primary reason for non-intensification of statin therapy.
Conclusion
Achievement of target LDL-C level is suboptimal in Korean patients with dyslipidemia, especially in those at very high-risk of CV events. Current practices in LMTs need to be improved based on precise CV risk evaluation posed by dyslipidemia. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Bempedoic Acid for Lipid Management in the Indian Population: An Expert Opinion
Jagdish Hiremath, J C Mohan, Prakash Hazra, JP S Sawhney, Ashwani Mehta, Sadanand Shetty, Abraham Oomman, Mahesh K Shah, Ganapathi Bantwal, Rajeev Agarwal, Rajiv Karnik, Peeyush Jain, Saumitra Ray, Sambit Das, Vibhuti Jadhao, Sachin Suryawanshi, Hanmant B
Cureus.2023;[Epub] CrossRef - Optimal implementation of the 2019 ESC/EAS dyslipidaemia guidelines in patients with and without atherosclerotic cardiovascular disease across Europe: a simulation based on the DA VINCI study
Julia Brandts, Sarah Bray, Guillermo Villa, Alberico L. Catapano, Neil R. Poulter, Antonio J. Vallejo-Vaz, Kausik K. Ray
The Lancet Regional Health - Europe.2023; 31: 100665. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Target Low-Density Lipoprotein-Cholesterol and Secondary Prevention for Patients with Acute Myocardial Infarction: A Korean Nationwide Cohort Study
Ju Hyeon Kim, Jung-Joon Cha, Subin Lim, Jungseok An, Mi-Na Kim, Soon Jun Hong, Hyung Joon Joo, Jae Hyoung Park, Cheol Woong Yu, Do-Sun Lim, Kyeongmin Byeon, Sang-Wook Kim, Eun-Seok Shin, Kwang Soo Cha, Jei Keon Chae, Youngkeun Ahn, Myung Ho Jeong, Tae Hoo
Journal of Clinical Medicine.2022; 11(9): 2650. CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - There is urgent need to treat atherosclerotic cardiovascular disease risk earlier, more intensively, and with greater precision: A review of current practice and recommendations for improved effectiveness
Michael E. Makover, Michael D. Shapiro, Peter P. Toth
American Journal of Preventive Cardiology.2022; 12: 100371. CrossRef - Non-achievement of the Low-Density Lipoprotein Cholesterol Goal in Older Patients with Type 2 Diabetes Mellitus and a Very High Cardiovascular Disease Risk: A Multicenter Study in Vietnam
Huan Thanh Nguyen, Khang Pham Trong Ha, An Huu Nguyen, Thu Thanh Nguyen, Hang My Lam
Annals of Geriatric Medicine and Research.2021; 25(4): 278. CrossRef
- Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement

- Thyrotropin Suppresses INF-r Mediated Gene Expression by Inhibiting Signal Transducer and Activation of Transcription 1(STAT1) Activity in FRTL-5 Cells.
- Min Ho Song, Young Kun Kim, Heung Kyu Ro, Eun Shin Park, Soon Hee Yoo, Ho Kim, Kang Wook Lee, Hee Jung Han, Won Chan Joo, Jin Ho Won, Kyu Lim, Oh Yoo Kwon
- J Korean Endocr Soc. 1998;13(4):536-553. Published online January 1, 2001
- 1,085 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The proinflammatory cytokine, IFN-y has been shown to exert pleiotropic effects in a variety of pathophysiologic conditions in autoimmune thyroid disease. The thyrocyte response to IFN-y is mediated two distinct classes of proteins, Janus kinases(Jakl and Jak2) and Signal Transducers and Activation of Transcription(STATl). The activation of STAT 1 is involved in the regulation of many interferon stimulated genes, such as MHC class II, intercellular adhesion molecules-1(ICAM-1) and MHC class II transactivator(CIITA) after the binding to the GASgFN- pactivated site) of the gene promoters. Recently we found TSH/forskolin inhibits IFN-y stimulated maximal expression of ICAM-1 in FRTL-5 cell. IFN-y action is localized between -175 bp and -97 bp from the start of translation of ICAM-1 gene which contains regulatory elements known to be involved in IFN-y action in other eukaryotic cells, palindromic IFN-y activated site(GAS)(5-TTTCCGGGAAA-3) which could bind STAT1, STAT3, STAT5, STAT6. Furthermore, the addition of TSH and forskolin causes a decrease in ICAM-1 promoter activity and its action was localized in GAS. These findings suggested TSH/cAMP signaling pathways downregulate IFN-y activated Janus kinase-STAT signaling path. We wanted to explore the possible involvement of elevated cAMP in the negative regulation of IFN-y induced STAT1 activation in thyroid cells. METHOD: We made several 5-deletion constructs of rat ICAM-1 promoter and analyzed the promoter activities by measuring the luciferase activity after tranfection into FRTL-5 cells. The protein/DNA complex was measured by electrophoretic mobility shift analysis using labeled oligonucleotide. We checked the level of total and phosphorylated STATl protein by immunoblot analysis using specific antibodies. RESULTS: Stimulation of IFN-y in FRTL-5 cells resulted in rapid activation of STATl/DNA binding activity, which was apparent after several minute of stimulation, maintains its activity until 48 h. Incubation of cells with TSH result in suppression of IFN-p mediated STAT1/DNA binding activity throughout the time course of activation by IFN-y. Addition of TSH into 5H maintained FRTL-5 cells did not change the total amount of latent STAT1 amount and also not affect IFN-y mediated production of total STAT1 until 4 h. IFN-y(100 U/mL) rapidly induced phosphorylation of STAT1 within 30 min. and maintained its level without significant change until 48 hours. Cells treated with TSH dramatically lowered the level of IFN-y induced production and phosphorylation of STAT1 after 12 h, 24 h, 36 h, and 48 h but TSH had no effect on the level of phosphorylated STATl within 4 h after IFN-y stimulation. The proteasome inhibitor, MG132 and phosphatase inhibitor, sodium orthovanadate did not block the TSH or forskolin mediated downregulation of phosphorylated STAT1. CONCLUSION: These results indicate a regulatory mechanism which TSH signaling can modulate the prolonged activation of Jak/Stat by IFN-y. We identified one of mechanisms related to TSH mediated negative suppression of the ICAM-1 gene; TSH/cAMP signaling pathways downregulate the cytokine activated Janus kinase-STAT signaling path.


 KES
KES

 First
First Prev
Prev



